Vitamin D In children
Vitamin D .
(cholecalciferol)
Vit. D2 (ergocalciferol ) derived from fungal and plant sources .
Vit. D3 (cholecalciferol ) is derived from
animal sources and is made in
the skin when 7;-dehydrocholesterol
reacts with UVB .
Mechanism
synthesis active form of vit .D .
 The liver and kidney help convert
vitamin D to its active hormone form , Once vitamin D is produced in the skin
or consumed in food , it requires chemical conversion in the liver and kidney
to form 1,25 dihydroxyvitamin D, the physiologically active form of vitamin D.
The liver and kidney help convert
vitamin D to its active hormone form , Once vitamin D is produced in the skin
or consumed in food , it requires chemical conversion in the liver and kidney
to form 1,25 dihydroxyvitamin D, the physiologically active form of vitamin D.
•
Active vitamin D functions as a hormone because it sends a message to
the intestines to increase the absorption of calcium and phosphorus .
•
IN VIT. D def. lessCa2 absorbed from the
intestine lead to decrease in s.Ca2 concentration leads to PTH secration which
lead to mobilazation of Ca and Ph from bone (to maintain Ca level ).
The major biologic function of vitamin D .
•
vitamin D helps to form and maintain strong bones.
•
Without vitamin D, bones can
become thin, brittle,or misshapen.
Vitamin D sufficiency prevents rickets in children
and osteomalacia in adults.
1)
Increase calcium absorption .
2)
Increase bone calcification and reabsorption
.
3)
Maintain calcium, phosphate and
bone homeostasis
sources of vitamin D
In the 1930s, rickets was a major public health problem in the (U.S.).
A
milk fortification program was implemented to combat rickets, and it nearly
eliminated this disorder in the U.S.
About 98% to 99% of the milk supply in the
U.S. is fortified with 10 micg (equal to 400 International Units or IU) of
vitamin D per quart.
One cup of vitamin D fortified milk supplies
one-half of the recommended daily intake for adults between the ages of 19 and
50.
Natural sources of vitamin D
What is the recommended intake for vitamin D?
Three important types of reference values
included in the DRIs (Dietary Reference Intakes) :
The Recommended Dietary Allowances (RDA)
recommends the average daily intake that is
sufficient to meet the nutrient requirements of nearly all (97-98%) healthy
individuals in each age and gender group.
Adequate Intakes (AI)
is set when there is insufficient scientific
data available to establish a RDA. AIs meet or exceed the amount needed to
maintain a nutritional state of adequacy in nearly all members of a specific
age and gender group.
The Tolerable Upper Intake Level (UL ) :
is the maximum daily intake unlikely to
result in adverse health effects
The recommended intake for vitamin D , cont,
Prevention of rickets :
exposure to ultraviolate light or by vit D
orally (400 iu daily ).
Treatment of rickets :
50-150micg vit.3 or 0.5-2micg 1,25
dihydroxcholecalcifero (2- wks ).
A single dose of 15,000micg of vit D
(without further therapy for several months )
The biological activity of 1 μg vitamin D
is equal to 40 IUs
The recommended intake for vitamin D , cont,
When can vitamin D deficiency occur ?
Nutrient deficiencies are usually the result of
dietary inadequacy, impaired absorption and utilization, increased requirement,
or increased excretion (loss).
1) when usual intake is below
recommended levels .
2) when there is limited exposure to sunlight
3) when the kidney cannot convert vitamin D
to its active hormone form.
4) when someone cannot adequately absorb
vitamin D from the digestive tract .
When can vitamin D deficiency occur ? cont,
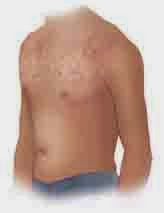
Diseases caused by deficiency
failure to mineralize growing bone
. leading to impaired growth (rickets dwarfism ), and deformity of the long bones ( bow legs , small
deformity pelvic ) delay teething ( caries ), delay stand and walk (lack of
muscle tone ).
C/signs : craniotabes ,forming prominence
(bosses ) ,thickening of wrist and ankle , rachitic rosary (chest ),delayed
closures A.F ,
a bone-thinning disorder that occurs
exclusively in adults and is characterised by proximal muscle weakness and bone
fragility.
Diseases caused by deficiency. Cont ,
a condition characterized by reduced bone mineral density and increased
bone fragility.
High blood pressure , T B , Cancer , periodental disease ,
multiple sclerosis , chronic pain , depression , schizophrenia , and several
autoimmune diseases including DM type 1 .
Who may need extra vitamin D to prevent a
deficiency?
1) Infants who are exclusively breastfed
(breast milk provides approximately 25 IU vitamin D/L ) .
Who may need extra vitamin D to prevent a
deficiency? Cont ,
2) Older adults.
As
people age, skin cannot synthesize vitamin D as efficiently and the kidney is
less able to convert vitamin D to its active hormone form .
3) Persons with limited sun exposure.
4) Persons
with greater skin melanin content.
5) Persons with fat malabsorption .
vitamin D requires some dietary fat for
absorption. Pancreatic enzyme deficiency , Crohn's Disease , Cystic Fibrosis ,
Celiac Disease , Liver disease وSurgical removal of part or all of the stomach
or intestines can impair digestion and absorption of many nutrients.
Other role of vit .D
evidence suggests that vitamin D may be protective against some cancers. Epidemiologic studies suggest that a higher dietary intake of calcium and vitamin D, and/or sunlight-induced vitamin D synthesis, correlates with lower incidence of cancer.
Research indicates that vitamin D plays a
role in preventing coronary disease. As with cancer incidence, the same
qualitative inverse correlations exist between coronary disease incidence and serum
vitamin D levels.
Other role of vit .D cont,
Corticosteroid medications such as prednisone have potential side effects, including decreased calcium absorption may also impair vitamin D metabolism.
Vitamin D and caffeine:
High caffeine intake may accelerate bone loss.
Caffeine may inhibit vitamin D receptors, thus limiting absorption of
vitamin D and decreasing bone mineral density. A study found that elderly
postmenopausal women who consumed more than 300 milligrams per day of caffeine
lost more bone in the spine than women who consumed less than 300 milligrams
per day .
What are the health risks of too much vitamin
D?
Vitamin D toxicity can cause nausea, vomiting,
poor apetite, constipation, weakness, and weight loss.
It can also raise blood levels of calcium
causing confusion. heart rhythm abnormalities. Calcinosis, the deposition of
calcium and phosphate in the body's soft tissues such as the kidney,
Sun exposure ,Diet are unlikely to cause
vitamin D toxicity, unless large amounts of cod liver oil are consumed.
Vitamin D toxicity is much more likely to occur
from high intakes of vitamin D in supplements.
Vitamin D toxicity( hypervitaminosis D)
over 500 micg /d for weeks = toxicity
over 500 micg /d for weeks = toxicity
Tolerable Upper Intake Level (UL) of vitamin D
for children and adults is 50 micrograms/day (2,000 IU/day).
Long term intakes above the UL increase the risk of adverse health
effects.
In adults, sustained intake of 2500
micrograms/day (100,000 IU) can produce toxicity within a few months .
For infants (birth to 12 months) the tolerable
UL is set at 25 micrograms/day (1000 IU/day), and vitamin D concentrations
of 1000 micrograms/day (40,000 IU) in infants has been shown to produce
toxicity within 1 to 4 months.
Vitamin D toxicity . Cont ,
THANK
YOU